It’s been true since Edward Jenner’s day: finding a vaccine is just the first step. Getting it out into the world demands a lot more problem-solving.
- 30 April 2024
- by Gavi Staff
On a recent morning – let’s say it’s this morning – in red-earthed or grassy or cinnamon-sanded villages; in harried, beeping towns of asphalt and cantilevered concrete; in neglected urban thickets, towers bowing as they rise; in one-roomed clinics, plastic sandals waiting obediently on the porch; or in neat structures behind well-pruned rows of flowering bushes; under the stretched shade of a wide tree, or in the black shadow of a cloud, or under the furnace blast of the desert sun, a fridge door opened.
Inside, a bulb zinged on, flinging light at the face of a health worker. She is the runner of the penultimate mile in a very long relay race that has been going non-stop since the mid-1970s.
The race’s route begins radial, sprung like spokes on a cart wheel, then branches off. The wheel-hubs are manufacturing plants. Airplanes fly out, to every country. In every country, a fine, fragile, but strikingly resilient capillary network leads onwards to almost every place that people live.
This is the vaccine cold chain. When you pause to think about it, it’s kind of incredible.
A very big, very global project
Since 1974, the world has saved 154 million lives with vaccination. That has required hundreds of thousands of pairs of hands, and hundreds of thousands of fridges, freezers and passive devices.
The absolute numbers are unknown. But we can tell you that since 2017 alone, Gavi, through its cold chain equipment optimisation platform (CCEOP) and COVAX, has helped procure:
- More than 37,000 ice-lined refrigerators and freezers;
- More than 45,000 solar direct-drive refrigerators and freezers;
- More than 200 walk-in cold rooms or freezer rooms; and
- More than 23,000 cold boxes
… to help shore up vaccine cold chains in more than 50 countries.
The health worker at the fridge door is peering at vials. Her job is to check, count, stock, stack, measure, record, maintain. She has both pen and paper, and automated monitoring tools on hand. It is necessary to be methodical: this work is both routine and life-or-death.
Vaccines are powerful, but finicky. All the vials in this fridge need to stay at temperatures between two and eight degrees Celsius. They have travelled all this way without ever dipping below or rising above that bracket. There’s still time for a stumble before the finish line, however. If that happens, they will lose their potency, and need to be discarded.
Next up is the handover. The runners of the final mile are waiting with blue vaccine carrier-boxes slung over their shoulders. Our health workers will fill their day’s inventory, and then they will leave here and travel – short distances or long, on foot, on bikes, in cars, in boats, on donkeys, ponies, camels, punting canoes or dodgy-looking rafts, past checkpoints, over skinny bridges, up ladders, and on and on – to a place where children need vaccines.
The relay race’s finish line and prize are the same: a child, immunised. The race repeats ceaselessly. Each year, approximately 134 million children are born vulnerable.
The problem of a stable vaccine
The smallpox vaccine was more than a century and a half old by the time, at the 11th World Health Assembly (WHA) in 1958, the delegate of the USSR called for the virus’s global eradication.
Countries that had managed to consistently get vaccines to their populations were already smallpox-free: the vaccine itself, in other words, worked well. But large swathes of the world map remained excluded from reliable access. In these places, people remained in danger – about 50 million cases of smallpox were occurring each year, globally – and the virus found a refuge from which it could spring future attacks.
A persistent difficulty, since the vaccine’s discovery in the late 18th century, had been transporting the immunising viral matter – a living substance – without it losing its potency.
The most reliable1 answer for a long time was to transport it in the body of a person, in a process called arm-to-arm vaccination. Described simply: a child was vaccinated with the cowpox virus, a mild virus naturally protective against its deadly cousin, smallpox; her immune response caused a pustule to form at the site of immunisation on her arm; before it healed, the matter from the pustule was taken, and poked into the next child.
Many, many children were protected in this way. But this distribution method had hefty logistical drawbacks. If you vaccinated too many children all at once, or found too few candidates, you risked breaking the chain – that is, not having an unhealed pustule to hand when you needed it for an unimmunised child.
If the vaccine needed to travel, a child needed to travel – and if the journey was a long sea voyage, you might need to arrange for a sequence of children to be ready on board. And even then, there was always a risk the vaccine didn’t take – no pustule, no more vaccine. Near-universal vaccination by these means would always have been a stretch.
By the mid-19th century, animals had been drafted into the vaccine supply chain. It worked like this: cowpox was inserted into a long scratch in the side of a calf, sheep or water buffalo, and four days later, lymph was harvested for use. In other words, vaccine lymph could now be farmed.
By 1900, it was common to add glycerine to prevent the transmission of bacterial infections along with the vaccine virus. Scientists showed that this process also helped vaccine stocks store better, though warmer weather compromised longevity.
Have you read?
Turn by turn, the vaccine was becoming a more regular and reliable product – but was still not stable enough to dependably weather long journeys. On the cusp of the 20th century, tubes of glycerinated calves’ lymph shipped from England were arriving in colonised Africa and Asia “useless” – a word used both by a governor of the Gambia and a surgeon in Uganda. Other packaging and preservation methods, ivory points ready-tipped with calf lymph, for instance, were trialled without breakthrough success. Establishing vaccine farms in, for example, East Africa, were considered as a solution, but, for complex and colonial reasons2, didn’t materialise.
A chilling proposal
But in the late 1940s, a London bacteriologist and virologist called Leslie Collier began to work on a freeze-dried version of the smallpox vaccine. “The glycerinated lymph produced in this country deteriorates rapidly at temperatures above 0°C,” he observed in a paper on his research in 1955. A more stable vaccine would prove “invaluable” for dispatch to regions without refrigeration, he wrote – and had discovered it. Sheep virus dried in 5% peptone “still gave a full quota of successful primary vaccinations of children under storage for 12 months at 22°C, or for 4 months at 37°C,” Collier reported.
Soon, health care workers in endemic countries would be able to carry the vaccine in their bags for as long as a month and still be able to deliver a protective jab. “Potent dried vaccine was an essential tool that could make the eradication of smallpox possible,” wrote Donald A. Henderson, chief of WHO’s eradication effort, looking back on Collier’s breakthrough from the threshold of triumph in 1976.
Freezing out smallpox
During the first ten years of the eradication mission, progress had been halting. “Of the countries where smallpox had been endemic in 1959, comparatively few had achieved smallpox-free status by the end of 1965,” recorded WHO in the 1968 publication The Second Ten Years of the World Health Organization. Moreover, Peru, formerly smallpox-free, was recording transmission again. “Failures in the various programmes were largely attributable to lack of transport and personnel and to inadequate supplies of freeze-dried vaccine,” diagnosed the authors.
A fresh push kicked off at the 1966 World Health Assembly, with a new emphasis on mass vaccination. In addition to what endemic countries were producing, 200 million doses of freeze-dried vaccine would need to be sent from abroad, experts estimated. The Soviet Union stepped up, providing 80% of the doses contributed to the effort through WHO.
Soon progress was bounding. In 1970, 18 countries reported endemic cases. By 1973, just Bangladesh, Ethiopia, India, Nepal and Pakistan were smallpox-endemic, and in October 1977, a young hospital cook in Somalia called Ali Maow Maalin became the world’s last smallpox patient.
Six more vaccines for six more diseases – back to the drawing board?
There were other vaccine-preventable diseases to worry about. By the time of the 1974 World Health Assembly, there was multilateral consensus that worrying about them collectively was a worthwhile endeavour.
Propelled in large part by the success of the smallpox programme – “a striking example of what can be done,” the WHO’s Director-General wrote in 1971 – the Expanded Programme on Immunization (EPI) called on Member States to “develop or maintain” immunisation and surveillance programmes against “diphtheria, pertussis, tetanus, measles, poliomyelitis, tuberculosis, smallpox and others, where applicable”. 3
The smallpox campaign would provide the rudimentary pattern: stepped vaccine distribution systems that mobilised existing health infrastructure, but were separated from the delivery systems for regular medicines. But, as the USSR’s delegate at the 29th WHA pointed out, there remained a “whole series of unsolved problems”. This project, first of all, would operate on a different kind of time-scale: continuous, open-ended.
Secondly, there was a still-unmet need for vaccines that would work well in tropical climates. Vaccines are biological products – each one is different. All but one of the first cohort of EPI vaccines were sensitive to heat, and some were sensitive to freezing. Unlike Collier’s stabilised smallpox vaccine, they wouldn’t tolerate a month in an off-the-grid health worker’s bag.
Would it be possible to safely store, transport and deliver them to children in hot countries with limited electricity networks? It was resolved that Ghana would play pilot and find out. In mid-1976, the west African country forged ahead.
Taking stock of the cold chain challenge
It became clear quickly that standard issue kitchen fridges weren’t going to cut it.
“Ambient temperatures in the field are often over 40°C and the power supplies for refrigeration are often unreliable or non-existent,” wrote WHO consultant John S. Lloyd in a 1977 report4 based on research conducted during the Ghanaian pilot. “In these conditions, domestic refrigerators and picnic boxes made in Europe are completely inadequate. Weakly constructed and usually damaged on delivery, these refrigerators are invariably under-insulated and under-powered; they also do not indicate the temperature and cannot be adapted to standby power facilities.”
Historical detour: consider the fridge
In purpose, and often in form, the fridge resembles its antecedent, the ice-box, but while one just stores naturally-occurring deposits of the cold, the other creates it by burning energy.
It was food, not biomedical biologicals, that people first sought to preserve in cool temperatures. Easy enough in winter – but in summer, or in warmer climates, that demanded innovation. As long ago as the third millennium BCE, a king called Shulgi from the city of Ur in Sumeria, boasted an ice-house. Science writer Tom Jackson suggests it may have been a hole in the ground, lined with timber for insulation, in which ice harvested in the mountains was stored.
In wealthier countries, like the USA, domestic iceboxes – cabinets made often of wood, lined with tin or zinc, cooled by a block of ice – were common by the end of the 1800s, at which point stored natural ice was also being used on the go, to preserve the catch on British fishing vessels. Ice-harvesting was a thriving industry.
But creating, rather than preserving, cold temperatures was an altogether different engineering challenge.
Artificial refrigeration via evaporative cooling was first demonstrated by William Cullen at the University of Glasgow, in 1748. He achieved this process by boiling ethyl ether in a partial vacuum. He didn’t, however, turn his discovery into an instrument. Over subsequent decades, other scientists tried alternative models, using alternative refrigerants. The first refrigerating machine to make it to market was based on compressed air, and sold by Alexander Twinning in 1856.
The first domestic fridge hit the American market in 1913, and was functionally an electrified refrigeration unit stacked on top of an ice-box. Early domestic fridges were expensive, with a 1922 model costing significantly more than a Model T Ford.
By 2007, about 1,300 million household fridges, and 350 million m3 of cold storage facilities are in use worldwide. In 2006, estimates pegged the global numbers of specialised refrigerated cargo ships at 1,300; refrigerated railcars at 80,000, refrigerated containers at 650,000 and refrigerated trucks at 1.2 million.
A functional, worldwide cold chain needed bespoke kit. At Korle-Bu, Accra, a national central vaccine store with flexible shelving space and variable temperatures ranging from -20°C to +4°C was called for. An alarm system should signal compressor failure, and a special, failsafe circuit should create a safety net for this largest and most valuable store of vaccines. Further, it needed a temperature recorder, and it needed to be used exclusively for vaccines, the WHO consultant wrote.
In their original condition, the regional stores were lacking, Lloyd found. The compression-type deep freezers used there lacked an alternative power source that could kick in during black-outs, and were so poorly insulated that they thawed within five hours when the electricity supply failed. Lloyd suggested better-insulated cabinets with a “permanent buffer store of ice” and a power source that could switch rapidly between electricity, gas or kerosene.
At the district level, 75-litre cold boxes packed out with ice from the regional store would keep a steady temperature for seven days, unopened. Generating cold, rather than keeping it, would prove more challenging. “At the district store there is, typically, no electricity supply or it is provided only intermittently,” Lloyd wrote. Kerosene-fuelled fridges would have to do – even if kerosene burners were “notorious for poor performance in Ghana, as in many other African countries”.
Lloyd’s analysis trickled down the branching chain to its last-mile tips. Vehicle-borne cold boxes would support a large number of daily vaccinations, but in the country’s north, vaccinators would proceed on foot from a temporary camp, and be limited to about 50 babies immunised each day.
But would the inoculating health worker know whether the vaccine would still be potent at that point? The expiry date of a vaccine is dependent not only on time, but also on temperature. Lloyd worried that manual recording was too easy to miss or mess up. “The most promising recent development in this field is an enzyme-based time/temperature indicator contained in a paper tab which is attached to the vaccine packet,” he wrote.
Ice-cold innovation
If Lloyd’s assessment in Ghana showed just how uphill the challenge was going to be, it wasn’t long before the hurdles were being chipped away.
Non-profit PATH set out to create the automated temperature recorders that Lloyd had identified as a worrying gap. An iterative process of invention produced, by the early 1990s, commercially-available vaccine vial monitors (VVMs): picture a sticker with a lilac target on it that changes colour as a signal of temperature failure. By 1999, these were a requirement on all vaccine vials purchased through the United Nations; in 2002 the Gavi Board required them for all vaccines purchased by the Vaccine Alliance from 2004 onwards.
Not only did the monitors provide health systems with confidence that no heat-damaged vaccines were being rolled out to children, but they massively helped to reduce waste. With the reassurance of the VVM, multi-dose vials could be used for more than one day, rather than being discarded, over-cautiously, at the end of an immunisation session.
Other temperature tracking tools have allowed health systems a more granular look at the weak spots in their cold chain. The Swiss company Berlinger & Co. AG, for instance, produces a 30-day temperature recorder (30DTR), a smart device that can report, in detail, on temperature fluctuations in larger vaccine stores.
Another vital invention – one that would quickly become the symbol of last-mile vaccine delivery – was the vaccine cold box. A first-generation, wooden version was created in 1974 by the National Bacteriological Laboratory of Sweden. Electrolux riffed on it, creating a transportable passive cold box that could remain cool for five days in 43°C weather.
But creating cold in hot weather, with scarce power, remained tricky. Absorption-type fridges that relied on kerosene, gas or electricity were preferred in developing countries, but they were bad at maintaining the required temperature ranges, and couldn’t freeze ice-packs at the volumes required to stock the passive cool boxes for vaccine transport. Moreover, fuel sources were often adulterated, leading to frequent breakdowns.
Better fridges were designed specifically for use in hotter climates. Lloyd’s call for a cold unit with a permanent ice buffer was met by the ice-lined refrigerator (ILR) – today, the standard choice for branches of the cold chain with unreliable power today. And, beginning in 1979, Electrolux created a line of small units especially for health centres, based on the portable cold box. These have remained in use for decades.
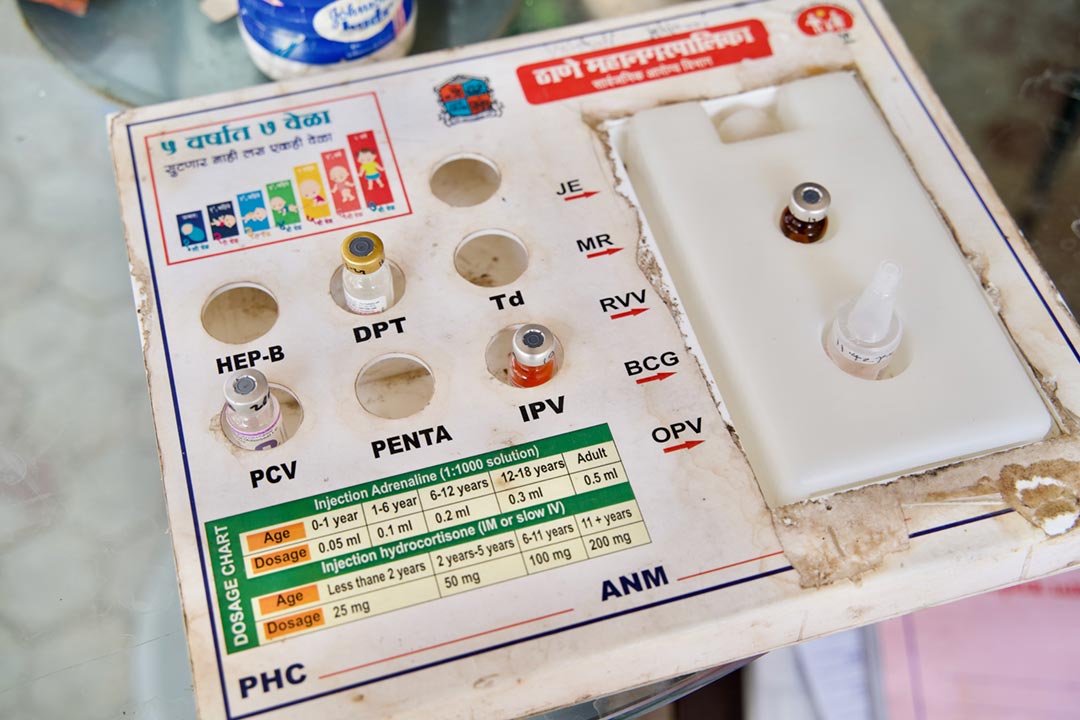
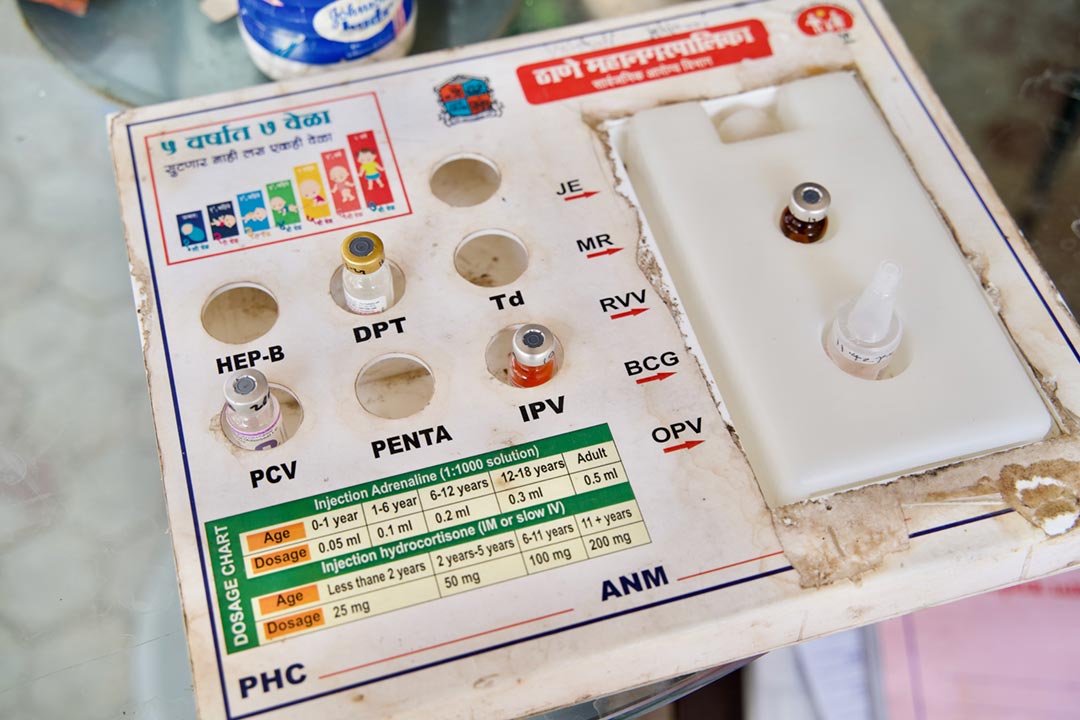
Credit: Gavi/2023/Prakhar Deep Jain
The cold chain continues to evolve. Even as many countries’ electrical grids have expanded and improved, national EPIs continue to upgrade their cooling tech to make use of cleaner, more reliable power sources – 50% of all the vaccine fridges installed by UNICEF in health systems around the world since 2017 are solar-powered.
Rome built roads, the EPI built the cold chain
Fifty years have passed since WHO Member States agreed that pursuing equitable immunisation deserved the considerable energy and ingenuity it would demand. The numbers vindicate that bet. Vaccination has saved 154 million lives since 1974. This year, a child under the age of ten is 40% more likely to survive to her next birthday than her counterpart, half a century ago.
It’s an achievement enabled by the effort of millions of people – parents, virologists and bacteriologists, government ministers, epidemiologists, solar power scientists, the health worker heaving open the door of the ILR, the vaccinator with his blue vaccine cooler box over his shoulder, the fridge technician and the solar-panel guy. The scaffold they’ve climbed on – and the built record of their collective exertions – is made of fridges and cooler boxes.
Zoom in: the cold chain in South Sudan
It’s the world’s least-electrified country, with dry-season temperatures tipping periodically into the 40s Celsius. There can’t be many places in which cold chain is more challenging to maintain, unbroken. And yet, South Sudan has managed to get vaccines to more children each year since 2016, reaching 76% of children with at least one jab in 2022. We asked our reporter in Juba, Winnie Cirino, to take a close look at how the country keeps its vaccines cool.
“The vaccines are cleared from the airport and moved into the National Vaccine Store,” Victor Sule, UNICEF Immunization Manager, told Cirino. “Records are taken after inspection and the reports of vaccine arrival are made, and then the vaccine is stored at the National Vaccine Store where there are a working cold room [and] working freezer room, for bulky vaccine storage.”
Then, each quarter, vaccines are distributed to South Sudan’s states, based on end-of-quarter reports on their inventory. For the 37 counties that are not reachable from state-level distribution due to poor roads or insecurity, vaccines are air-dropped from the national level.
In many counties, solar-powered fridges have made a massive difference. Counties like Mingkaman, which still rely on generator-run fridges, are like a glimpse back in time to the days when kerosene or gas-run cold chain tech were the only option in many places. Daniel Achop, the EPI County Officer at Mingkaman County Cold Chain told Cirino, “We are using a generator for the EPI services. If it goes off, like now, there is nothing we can do. The partner providing us with fuel says they don’t have enough fuel now,” Achop says. They’ve moved the vaccines into the primary health centre, he reports, but space in the facility’s cold storage is tight, and the risk of dose wasting is clearly a worry.
References
- Edward Jenner himself (Jenner pioneered the concept of vaccines and created the smallpox vaccine) suggested shipping dried cowpox lymph between two plates of glass, then rehydrating it with water at the destination. Unfortunately, this method failed often. Other early vaccinators carried lymph in its fluid state, in the tip of a lancet – but in this form, it lasted for two or three days at maximum. Already in Jenner’s lifetime it was clear that getting the lymph to hot climates would be even more challenging than transporting it within temperate Europe – though by 1802 at least one effort to ship usable lymph to India had worked. Historian of science and medicine Andrea Rusnock has more on these fascinating early efforts to establish a vaccine transport network.
- Historian Kristin Brig-Ortiz, interviewed by VaccinesWork here, has worked on this.
- WHA30.53, adopted in 1977, set out objectives for the EPI: “to immunize all children of the world by 1990, particularly against diphtheria, pertussis, tetanus, measles, poliomyelitis and tuberculosis, and reduce morbidity and mortality from other selected diseases of public health importance for which safe and effective vaccines currently exist or become available.”
- John S. Lloyd (1977) “Improving the cold chain for vaccines,” WHO Chronicle 31: 13-18.
This article was originally published on
VaccinesWork
